Answer
Premature ventricular contraction
Explanation:
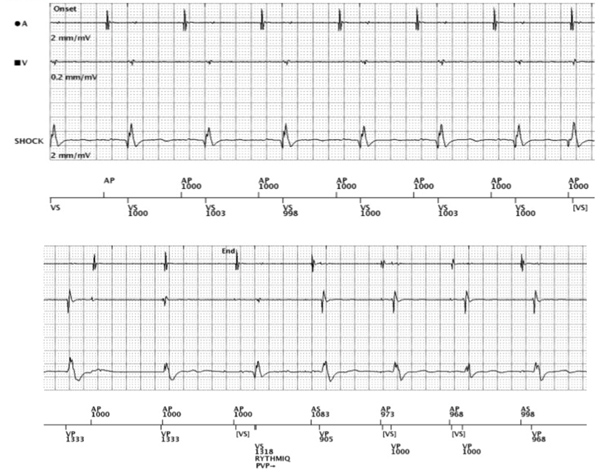
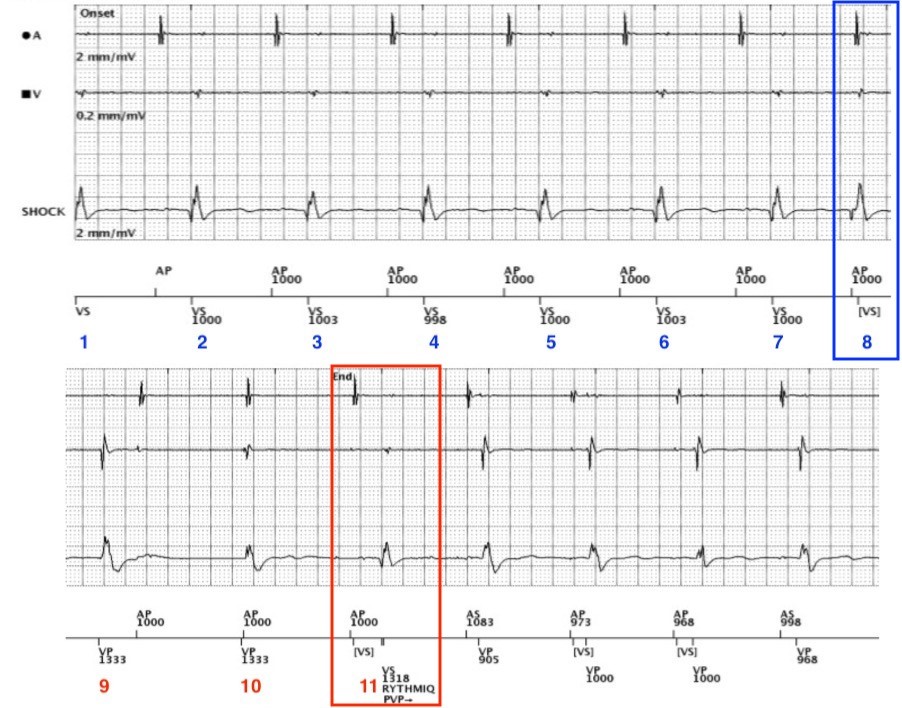
Figure 2: An annotated RYTHMIQ EGM illustrating the mechanism for device mode switch
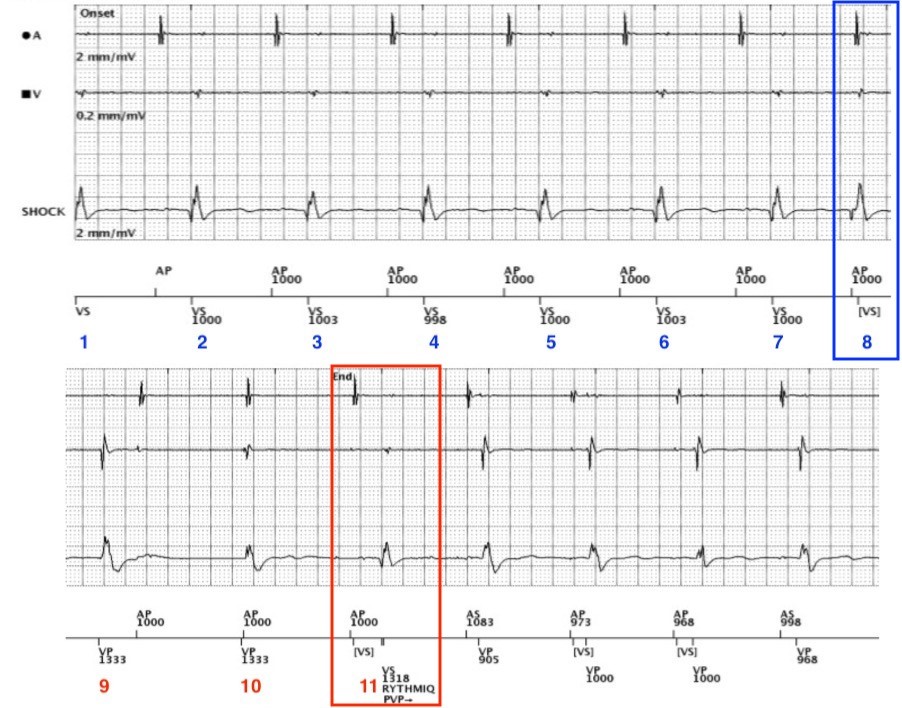
This recorded RYTHMIQ episode, illustrates normal device function in the context of a loss of atrioventricular synchrony. The aetiology of this episode demonstrating transition from acute arterial insufficiency (AAI), (VVI backup), to DDD pacemaker was an unfortunately timed premature ventricular contraction (PVC).
In this trace from left to right, we can see atrial demand pacing at a lower rate limit (LRL) of 1000 ms / 60 bpm. Intrinsic conduction appears prolonged, with measured PR intervals ranging from 280 ms to 320 ms.
At beat number eight, (as indicated in the blue box in Figure 2), we can see an uncharacteristically short A-V interval, with the ventricular event falling in the post-atrial ventricular blanking period. It would be notably impossible for this to be a conducted ventricular event, as we know the patient has a marked first-degree AV block at rest. The interval between atrial pace (AP) and VS is non-physiological and therefore can only be as a result of an ectopic beat or non-cardiac signal. We can see that the ventricular-sense (VS) marker in Figure 2 aligns with a QRS complex, with a subtly different morphology noted on both the ventricular and shock EGM channels; suggestive of ectopic ventricular origin.
This is an example of Boston Scientific’s RYTHMIQ algorithm, designed to minimise unnecessary ventricular pacing and prevent deleterious effects in patients with intact AV conduction.1,2 Unlike competitive algorithms, RYTHMIQ provides back-up VVI pacing at 15 bpm below the lower rate limit (LRL); in this case 1333 ms / 45 bpm.
When the device is programmed to RYTHMIQ, it will automatically switch to DDD(R) when three out of 11 ventricular beats are considered as ‘slow’.3
Slow ventricular beats include:4
- ventricular paced event;
- ventricular sensed event (lower rate limit + 150 ms);
- ventricular sensed event (sensor indicated rate + 150 ms).
In this example, the PVC precludes native intrinsic conduction at beat eight, which subsequently allows the ventricular LRL to timeout and deliver back-up asynchronous ventricular pacing (VP). The refractoriness of the ventricle post-VP precludes further AV conduction, leading to three slow asynchronous ventricular beats; thus, triggering DDD(R) mode at beat eleven (as indicated in the red box in Figure 2).
Following the eleventh beat, we can see synchronous atrial and ventricular pacing in the DDD(R) mode.
This case demonstrates normal, yet inappropriate, device behaviour for this patient. Although not well documented within the literature, PVC’s have been found to cause approximately 21% of inappropriate RYTHMIQ mode switches.5 Other causes of inappropriate RYTHMIQ mode transition include ventricular under-sensing, functionally non-conducted atrial events and isorhythmic AV dissociation.
Management:
Due to the correlation of pre-syncopal symptoms with RYTHMIQ episodes, we decided that a permanent DDDR mode with search AV+ would prevent future bradycardic events, whilst encouraging native intrinsic conduction in this patient.6 All other device settings were unchanged.
This case teaches us that ventricular tachyarrhythmias are not always the cause of pre-syncope/syncope in ICD patients. It also highlights the importance of appropriate patient selection for specific algorithmic programming.
References
- Carsten I. Pacing-induced heart failure: should we avoid right ventricular pacing or not?,EP Europace 2007;19(2):165–168. https://doi.org/10.1093/europace/euw316.
- Sweeney MO, Hellkamp AS, Ellenbogen KA, et al. Adverse effect of ventricular pacing on heart failure and atrial fibrillation among patients with normal baseline QRS duration in a clinical trial of pacemaker therapy for sinus node dysfunction. Circulation 2003;107(23):2932-2937.
- Bastian D and Fessele K. Strategies and pacemaker algorithms for avoidance of unnecessary right ventricular stimulation. In: Roka A. Current issues and recent advances in pacemaker therapy. London: InTech. https://doi.org/10.5772/48747.
- com. Pacing Modes Specific For Boston Scientific. 2020. https://www.cardiocases.com/en/pacingdefibrillation/specificities/pm-pacing-modes/boston-scientific/pacing-modes-specific-boston (Accessed 23 August 2020).
- Strik M, Defaye P, Eschalier R, et al. Performance of a Specific Algorithm to Minimize Right Ventricular Pacing: A Multicenter Study. Heart Rhythm 2016;13(6):1266-1273. https://doi.org/10.1016/j.hrthm.2016.02.008.
- The David Trial Investigators. Dual-chamber pacing or ventricular backup pacing in patients with an implantable defibrillator. The dual chamber and VVI implantable defibrillator (DAVID) trial.ACC Current Journal Review 2003;12(2):88.