Answer
Shorten AV delay
Explanation
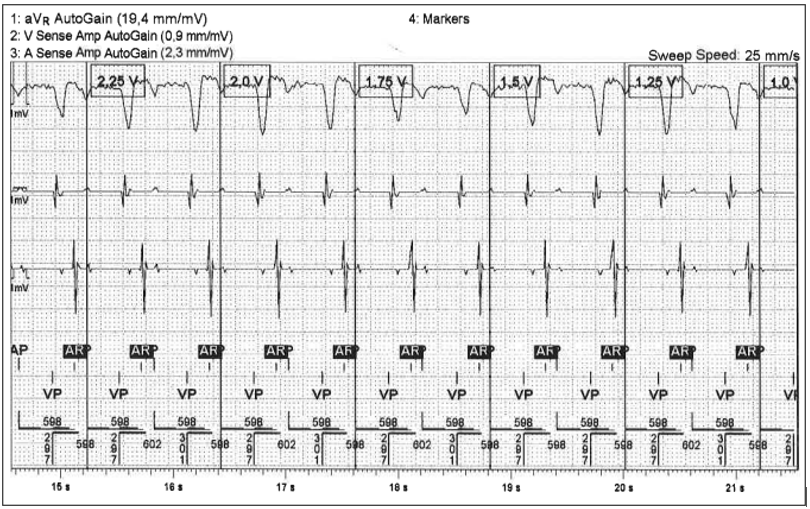
Figure 1 displays the trace recorded during the atrial threshold test. The trace starts with an atrial paced (AP) event followed by an AV delay of 300 ms and then a ventricular paced (VP) event. The next atrial event is marked as an atrial refractory (AR) event as it falls in the post ventricular atrial refractory period (PVARP). This event is a retrograde P wave. The long AV interval has allowed the atrium to be receptive to V-A conduction. As this event falls in the PVARP it does not affect timing cycles, with the next AP stimulus delivered as the atrial escape interval times out. This AP occurs in the absolute atrial refractory period, with the atrium having already been excited and does not capture. This pattern repeats at the test rate of 100 bpm until the atrial threshold test is stopped and does not allow for the measuring of an atrial threshold.
The reason for the sequence seen is the long AV interval. In Abbott pacemakers the default AV interval during manual atrial capture tests is 300 ms and it is therefore important to shorten this interval when performing an atrial threshold test especially if VA conduction is present. Hence the correct answer is shortening the AV delay.
Why it’s not the other options?
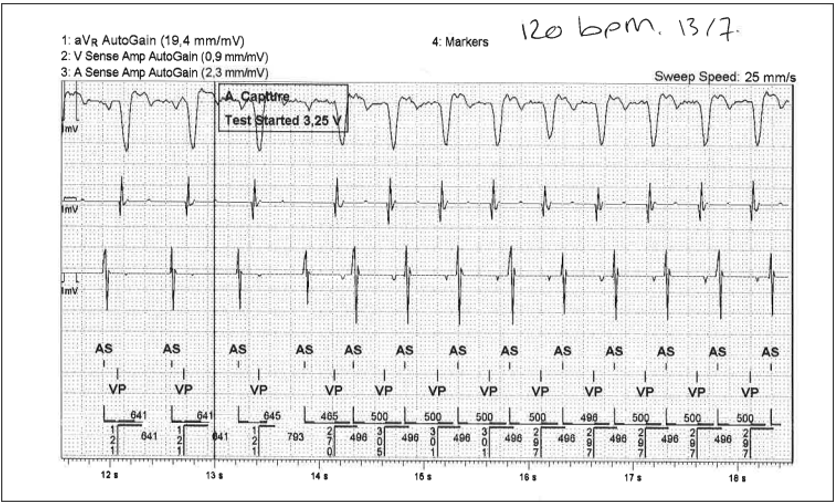
Increasing the test rate can be a useful way to measure an atrial threshold, especially when there is atrial ectopics hindering the test, however in this patient that was not the case. Figure 2 displays the atrial threshold test with the rate increased to 120 bpm but with no change to the AV interval. Here the test fails as atrial pacing is unable to be delivered. The retrograde P waves are falling outside of the PVARP and are sensed and tracked inhibiting atrial pacing.
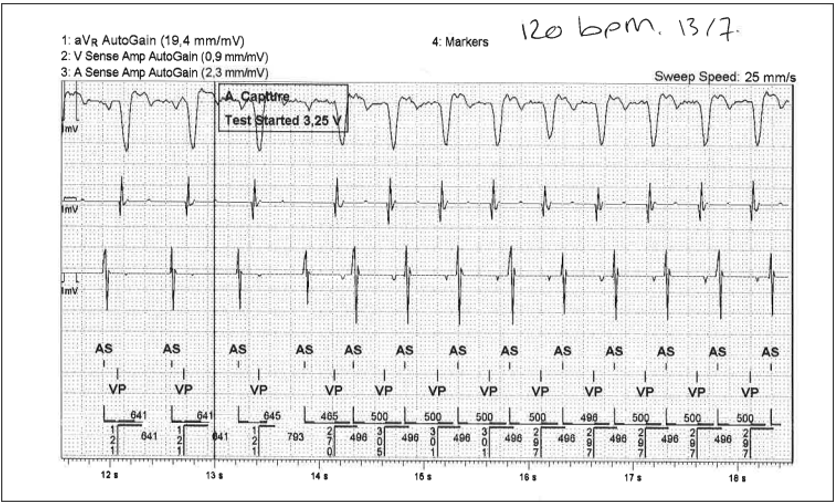
Figure 2: Electrogram recorded during an atrial threshold test in DDD mode at 120bpm. Channels top to bottom, 1. ECG channel aVR, 2. Ventricular sense amplitude EGM, 3. Atrial sense amplitude EGM, 4. Marker channel.
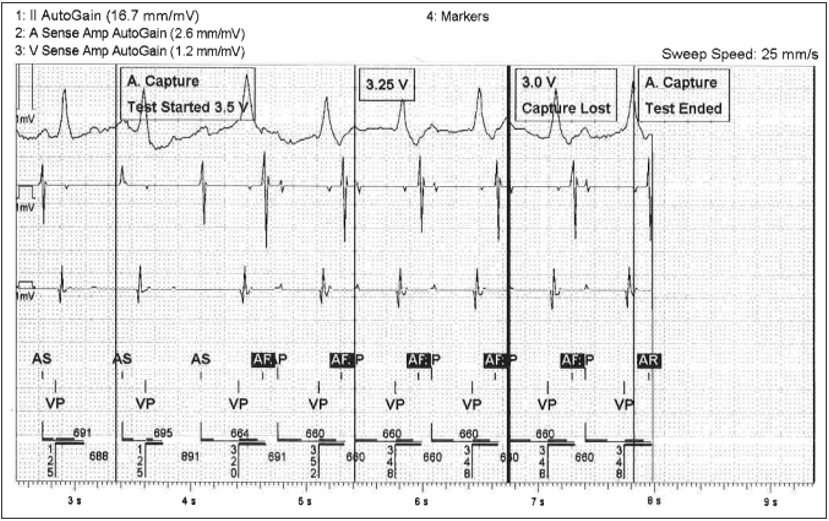
Decreasing the test rate did not help in this situation. A threshold test was performed at 90 bpm during a period where the sinus rate had reduced. The long AV interval still resulted in VA conduction and the inability to perform the test. (See figure 3)
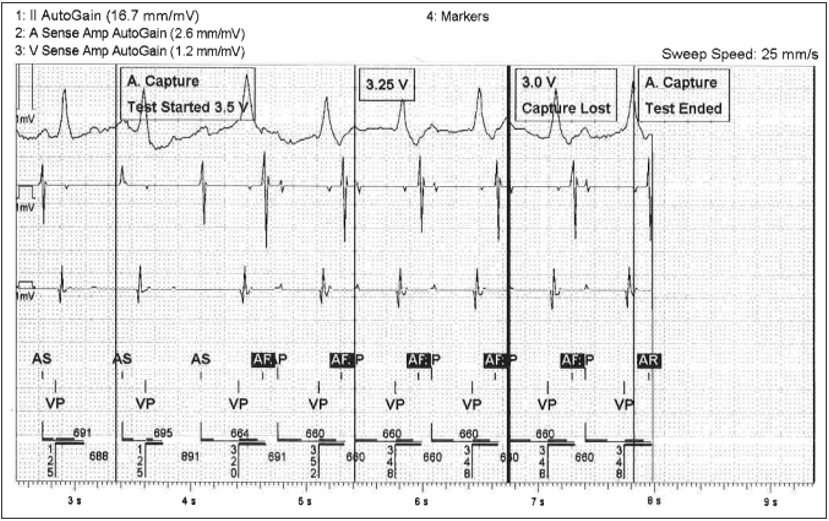
Figure 3: Electrogram recorded during an atrial threshold test at 90bpm. Channels top to bottom, 1. ECG channel Lead II. 2. Ventricular sense amplitude EGM. 3. Atrial sense amplitude EGM. 4. Marker channel.
Mode change. Changing the mode to AAI was not possible here as the history indicated CHB and there was no underlying AV conduction at 40 bpm.
Increasing the PVARP. Increasing the PVARP would have no impact on the retrograde P waves as they are already falling in the PVARP marked as an AR.
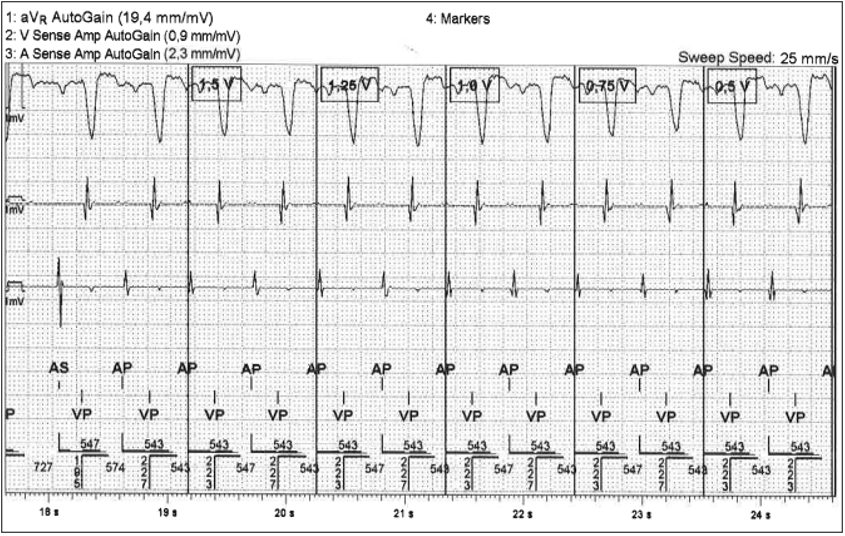
The final result is shown in figure 4 with a shortened AV delay of 230 ms. In this example due to a slight increase in atrial rate the test was performed at a rate of 110 bpm and an atrial threshold was successfully obtained.
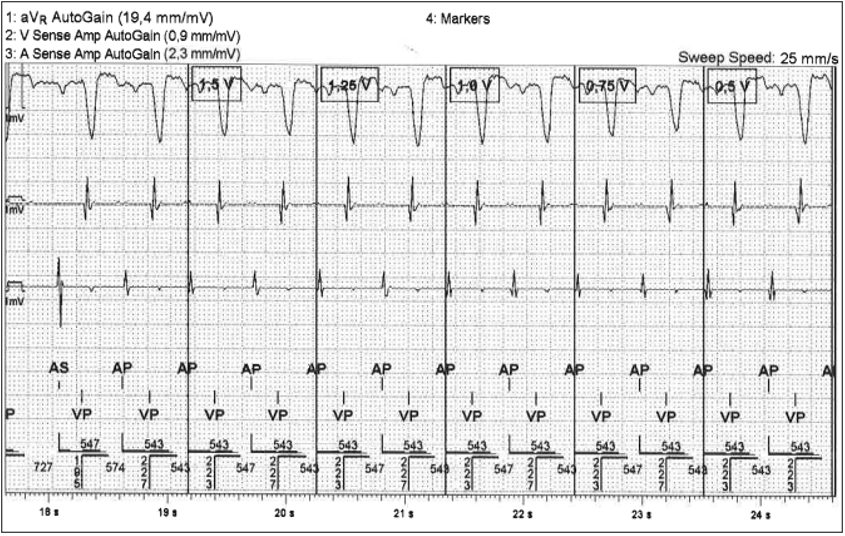
Figure 4: Electrogram recorded during an atrial threshold test following setting adjustments. Channels top to bottom, 1. ECG channel aVR, 2. Ventricular sense amplitude EGM, 3. Atrial sense amplitude EGM, 4. Marker channel.
Learning points
- Atrial threshold tests performed in DDD mode can be challenging in the presence of VA conduction, especially when a long AV interval is programmed.
- Knowledge of manufacture default test settings is useful when troubleshooting atrial capture tests.
- Shortening the paced AV delay will help in these scenarios by shortening the window for retrograde conduction to occur allowing for an atrial threshold to be obtained.