Answer
T wave oversensing.
Explanation
The ECG displayed is an example of post pacing T wave oversensing causing intermittent CRT-pacing during exercise. The ECG shows a regular atrial (sinus) rhythm at approximately 80 bpm. P waves are followed by a short AV interval (90 ms sensed AV interval) and LV paced complexes (appropriately tracked) or a longer PR interval and narrow intrinsic QRS complex (are not tracked) in a bigeminal pattern.
Of the options available there are only two answers which could explain the interrupted tracking of intrinsic P waves. Atrial undersensing or T wave oversensing which is causing, functional atrial undersensing. The text reports that atrial measurements were satisfactory and the atrial sensitivity threshold of 0.3 mV is an appropriately selected value for atrial sensing therefore the most likely explanation is T wave oversensing.
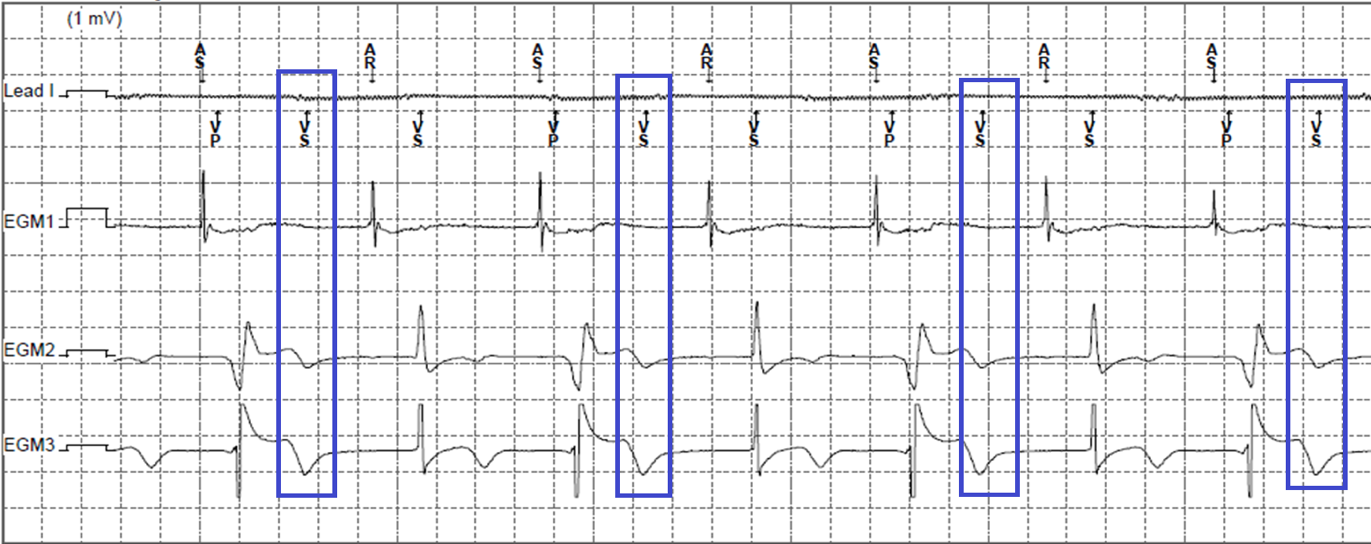
Figure 2 shows the EGM recorded at the time the ECG was recorded confirming post pacing T wave oversensing. The first event seen on the EGM shows atrial sensing (AS) ventricular pacing (VP). Note VP is LV pacing as per the described settings and there is a short AV interval as programmed. Following VP the next event is a ventricular sense (VS) which lines up with the post paced T wave (highlighted with the blue boxes). The VS (over-sensed T wave) triggers a post ventricular atrial refractory (PVARP) period which results in the next atrial event which falls in the PVARP being ignored, not tracked. The non-tracked atrial event conducts to the ventricle with a prolonged PR interval which gives rise to the intrinsic narrow QRS. The next event is tracked appropriately but the post paced T wave is again over-sensed and the sequence repeats.
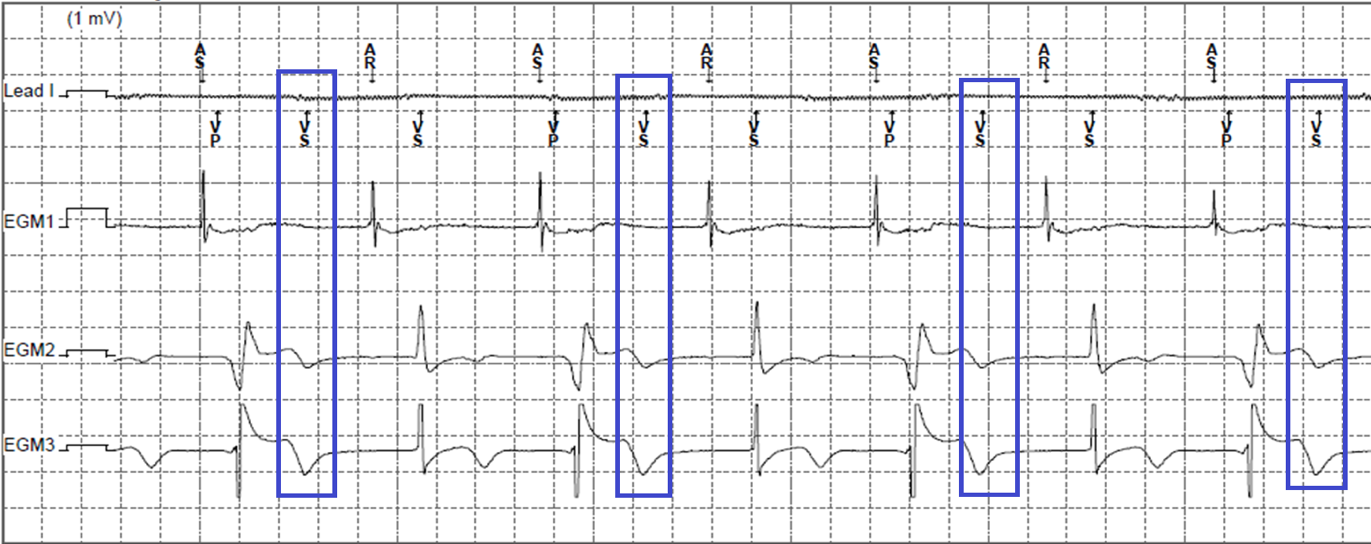
Figure 2
EGM stored simultaneously to the recorded 12 lead ECG. Lead I has no ECG attached but displays the marker channel. EGM 1 shows the atrial electrogram. EGM 2 shows the RV bipolar electrogram. EGM 3 shows the LV1 to RV coil electrogram. Blue boxes highlighting post pacing T wave oversensing
There are several methods of correcting post paced T wave oversensing. Some of these included;
• Decreasing the RV sensitivity
• Changing the LV pacing vector to a bipolar vector rather than an extended bipolar configuration
• Turn PVARP extension on PVC off (Does not solve T wave oversensing but would stop the second complex falling in AR, therefore alternate P waves would be tracked by the device)
• Changing the sensing vector from bipolar to RV tip to RV coil (integrated bipolar) which would only be possible if a dedicated lead was in situ.
In this particular situation, the patient was part of a research trial which would not allow a change to the LV pacing vector. The sensing vector was changed from bipolar to RV tip to RV coil. This caused a reduction of post pacing T wave oversensing but did not completely solve the situation. Consequently, the RV sensitivity was also decreased from 0.3mV to 0.45mV which resolved the issue.
Post pacing T wave oversensing is one of the many causes of reduced CRT pacing therapy. During a device check there might not be any clear evidence of T wave oversensing as the T wave oversensing has to appear consistently beat to beat to be recorded as an episode or you have to observe it occurring. One method of checking if there is post pacing T wave oversensing occurring on a device with reduced CRT pacing therapy is to exercise the patient as T waves can change during exercise.