Answer
Urgent cardiac catheterization followed by revascularization
Explanation/Discussion
The first ECG on arrival to ED (Fig 1A) showed polymorphic ventricular tachycardia. Following the first defibrillation and successful resuscitation, the subsequent ECG (Fig 1B) shows a wide QRS rhythm with diffuse ST elevation in leads I, AVL, and V4 to V6 with an interesting “Shark fin” morphology due to the fusion of QRS, ST-segment, and T waves. This can be easily mistaken for monomorphic tachycardia, the sine wave pattern of hyperkalemia, and tombstone appearance. Sharkfin appearance denotes transmural ischemia of a large territory in occlusion MI and hence occurs in specific leads correlating with coronary anatomy. The sine wave changes in hyperkalemia are a gradual process showing generalized changes in all ECG leads and correlate with rising potassium levels. The tombstone appearance in MI is seen more frequently than the sharkfin, has absent or minimal r wave duration (<0.04s) and amplitude, with convex ST elevation merging with T wave. In contrast, a gigantic R wave (>amplitude > 1 mv) is a characteristic of shark fin appearance, due to which it is known as a giant R wave pattern. (1)
Clinical Course
Echocardiography showed severe hypokinesia in the entire left anterior descending artery territory with an ejection fraction of 25-30%. The patient was taken for urgent coronary angiography, which revealed thrombotic occlusion in the proximal LAD. Successful primary angioplasty was done with mechanical circulatory support. The patient was stabilized after a few days and discharged in a hemodynamically stable state.
Discussion:
The shark fin pattern is an uncommon ECG sign seen in 1.4% of all STEMI patients and is an ominous sign that is often associated with poor outcomes. The precise pathophysiological mechanism for the pattern is still unknown. Some plausible mechanisms described are sudden total deprivation of blood flow to large areas of viable myocardium causing acute dilatation of LV cavity (Brodie`s hypothesis) and differential response of ischemic myocardium due to genetic variations in Ito, IK, Katp, and INa activity. (2,3)
Although described variedly in literature as a giant R wave pattern, lambda pattern, or triangular QRS-ST-T waveform pattern it does not confer the clinical significance of this important sign. Clinically shark “Shock” fin is a forewarning for impending cardiogenic shock and or cardiac arrest due to ventricular tachycardia/fibrillation. Interestingly this pattern degenerates into a shockable rhythm which has a better survival rate compared to pulseless electrical activity. Hence all medical personnel including the emergency physician, nurses, paramedics, and cardiologist should be forearmed to tackle two shocks
- Cardiogenic shock with a low threshold for using mechanical circulatory devices (IABP, ECMO, Impella)
- DC Shock/ defibrillation to revert shockable ventricular arrhythmias.
Take-home points:
- The Shark Fin pattern is an ominous ECG sign of occlusion myocardial infarction associated with cardiogenic shock and ventricular arrhythmia. It can be confused with hyperkalemia, ventricular tachycardia, and tombstone pattern.
- Treating team should take it as a forewarning for impending complications and be forearmed with MCS and DC shock/defibrillation to save the life of the patient.
References
- Balci B. Tombstoning ST-Elevation Myocardial Infarction. Curr Cardiol Rev . 2009 Mar 10 [cited 2023 Jul 29];5(4):273–8.
- Cipriani A, D’Amico G, Brunello G, Perazzolo Marra M, Migliore F, Cacciavillani L, et al. The electrocardiographic “triangular QRS-ST-T waveform” pattern in patients with ST-segment elevation myocardial infarction: Incidence, pathophysiology and clinical implications. J Electrocardiol. 2018 Jan 1;51(1):8–14.
- Jaiswal AK, Shah S. Shark Fin Electrocardiogram: A Deadly Electrocardiogram Pattern in ST-Elevation Myocardial Infarction (STEMI). Cureus . 2021 Jun 28 [cited 2023 Jul 29];13(6).
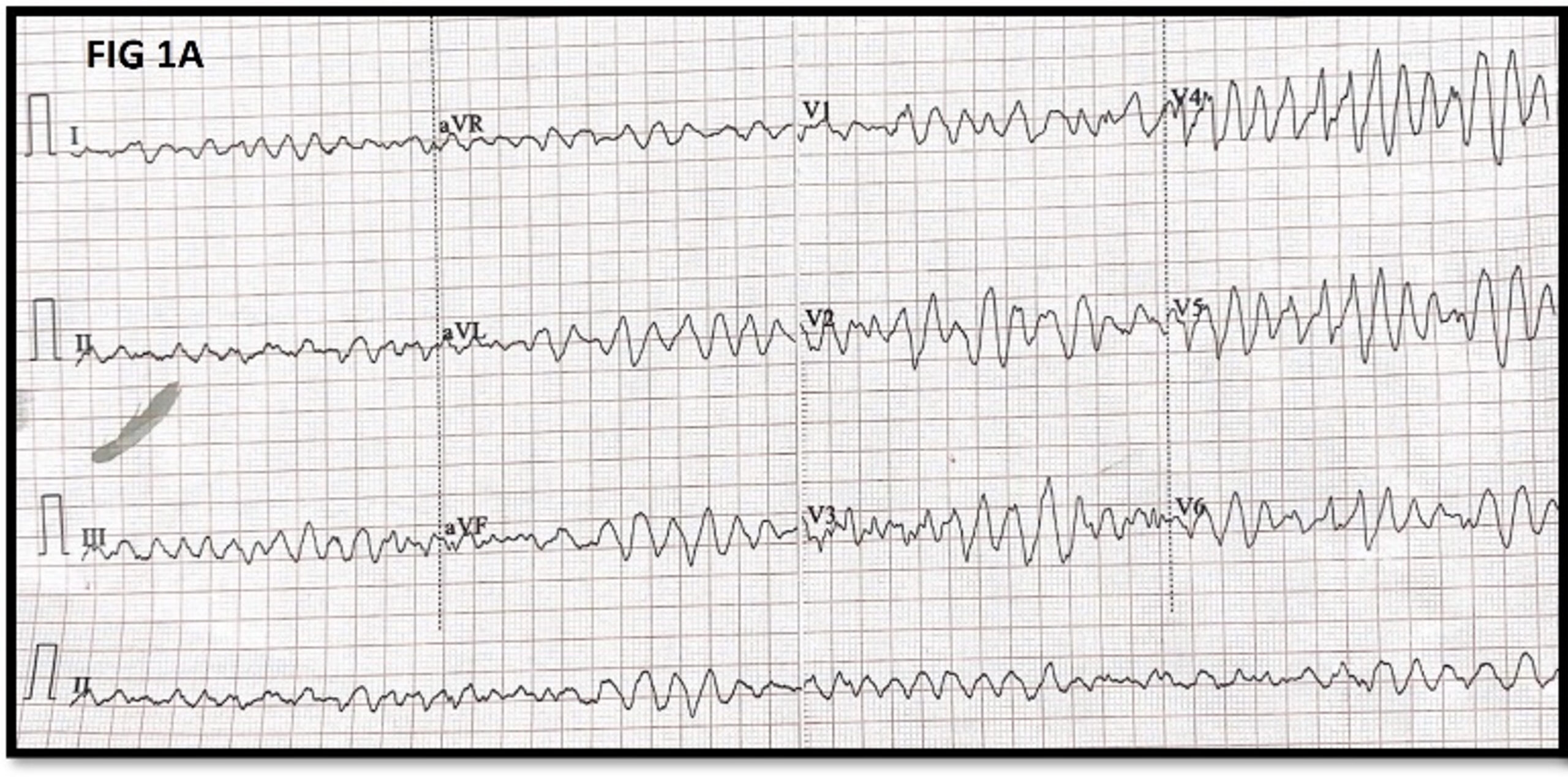 Figure 1 A- 12 lead ECG on arrival to ER
Figure 1 A- 12 lead ECG on arrival to ER

