March 2019
An unscheduled remote transmission received for ‘shock delivered’
Claire O’Neill – Advanced Specialist Cardiac Physiologist
Manchester University NHS Trust
Background
An unscheduled remote transmission was received from a 65-year-old male with a primary prevention single chamber ICD for ‘shock delivered’. Figure 1 shows the presenting EGM. Figure 2 shows the stored shock episode, which occurred when the patient had stood up to get out of bed earlier that morning. The patient’s history includes hypertrophic cardiomyopathy with poor LV systolic function, permanent atrial fibrillation, hypertension, chronic kidney disease, TIA and a previously treated LV apical thrombus. The ICD had been implanted six months prior to the transmission. The implant report states the procedure was uncomplicated, with an active fixation single coil RV lead placed on the low RV septum with satisfactory parameters. Programmed settings and recorded lead measurements are displayed below.
Mode: VVI
Lower rate: 40bpm
Therapy zone: VF only 200bpm, 30/40 intervals to detect
R wave measurement: 1.3mV
RV lead impedance: 342 ohms, stable trend
RV sensitivity 0.3mV
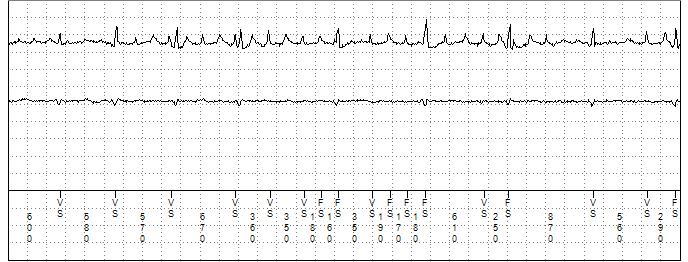

Figure 1
The presenting EGM seen on the remote transmission. Channel 1 displays the near field RV tip to RV ring EGM. Channel 2 a far field Can to RV coil EGM. Channel 3 the marker channel.

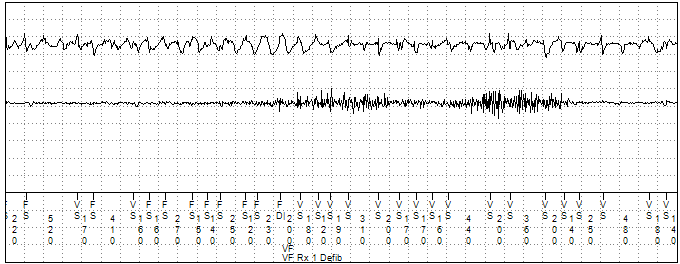


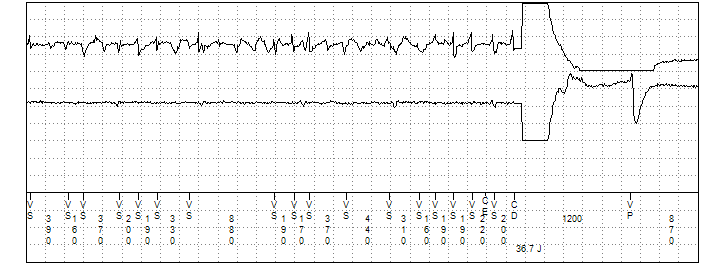
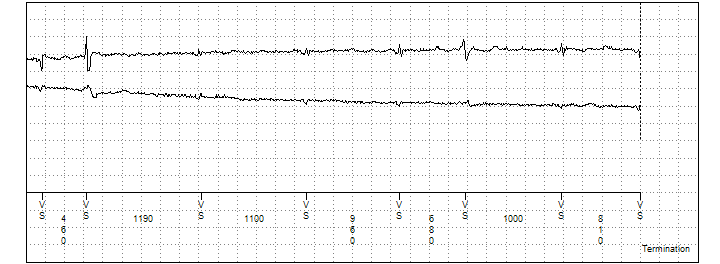
Figure 2
The remote transmission stored shock therapy episode. Channel 1 displays the near field RV tip to RV ring EGM. Channel 2 a far field Can to RV coil EGM. Channel 3 the marker channel.


.png)