March 2023
Ventricular vs. Supraventricular Broad Complex Tachycardia
Lana-Faye Anderson Trainee Clinical Cardiac Scientist, King’s College Hospital NHS Foundation Trust, UK
Disclosure: The author has no conflict of interests to declare.
Background
A 74 year old female presented to the emergency department with a 3 day history of left sided chest pain at rest, palpitations, shortness of breath on exertion and orthopnoea. Patient history revealed previous inferior myocardial infarctions in 1990 and 2021, which were treated with stents, as well as hypercholesterolemia and hypertension for which she was prescribed relevant medication. The 12-lead ECG below was recorded in the emergency department (Figure 1).
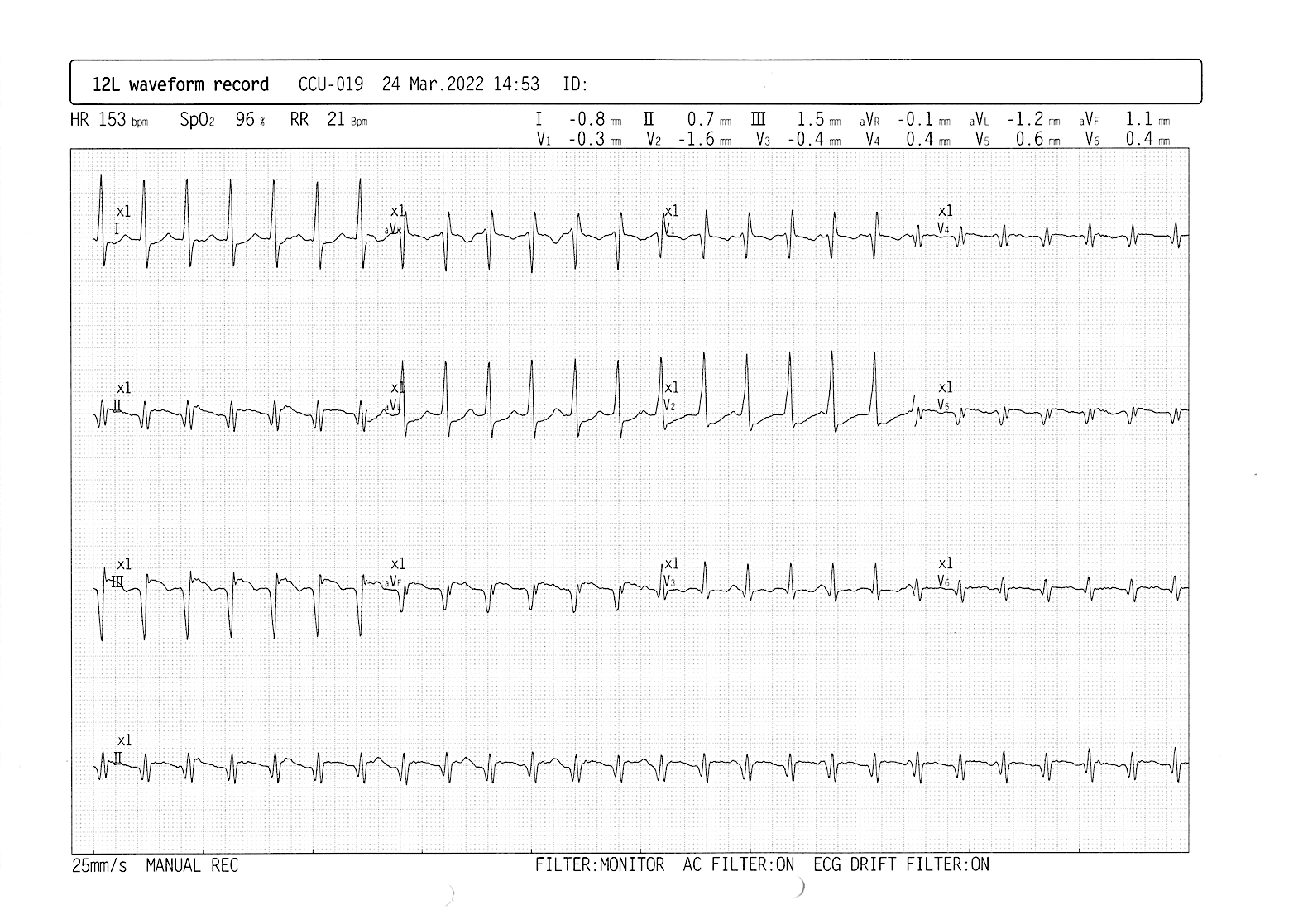
Figure 1. 12-lead ECG recorded in the emergency department
QUESTION
What is the correct interpretation of the ECG?
Sinus tachycardia
Supraventricular tachycardia with aberrancy
Antidromic atrioventricular re-entrant tachycardia
Monomorphic ventricular tachycardia
Answer
Monomorphic ventricular tachycardia
Explanation
The ECG shows broad complex tachycardia with a QRS complex duration of 128ms at a rate of 153bpm. Narrow complex tachycardia refers to a tachycardia with a QRS duration of £120ms, whilst broad complex tachycardias have a QRS duration of >120ms. Narrow complex tachycardias involve rapid activation of the ventricles via the His-Purkinje system, with the origin of the arrhythmia arising above or within the His bundle. Broad complex tachycardias are typically ventricular in origin, with ventricular tachycardia (VT) accounting for 80% of cases. However, in one fifth of patients, broad complex tachycardia characterises a supraventricular tachycardia (SVT) conducted with aberrancy (due to pre-existing or rate-related bundle branch block) or an SVT with antegrade conduction over an accessory pathway (such as in antidromic atrioventricular re-entrant tachycardia [AVRT]), which account for 15% and 5% of cases respectively. There is often difficulty in distinguishing between broad complex tachycardias of ventricular and supraventricular origin, resulting in up to 10% of cases being misdiagnosed.1
The correct diagnosis of broad complex tachycardia is critical for appropriate management. To help determine the origin of broad complex tachycardia, Brugada and co-workers published the Brugada algorithm, a stepwise decision-tree that considers 4 criteria for VT (Figure 2).2
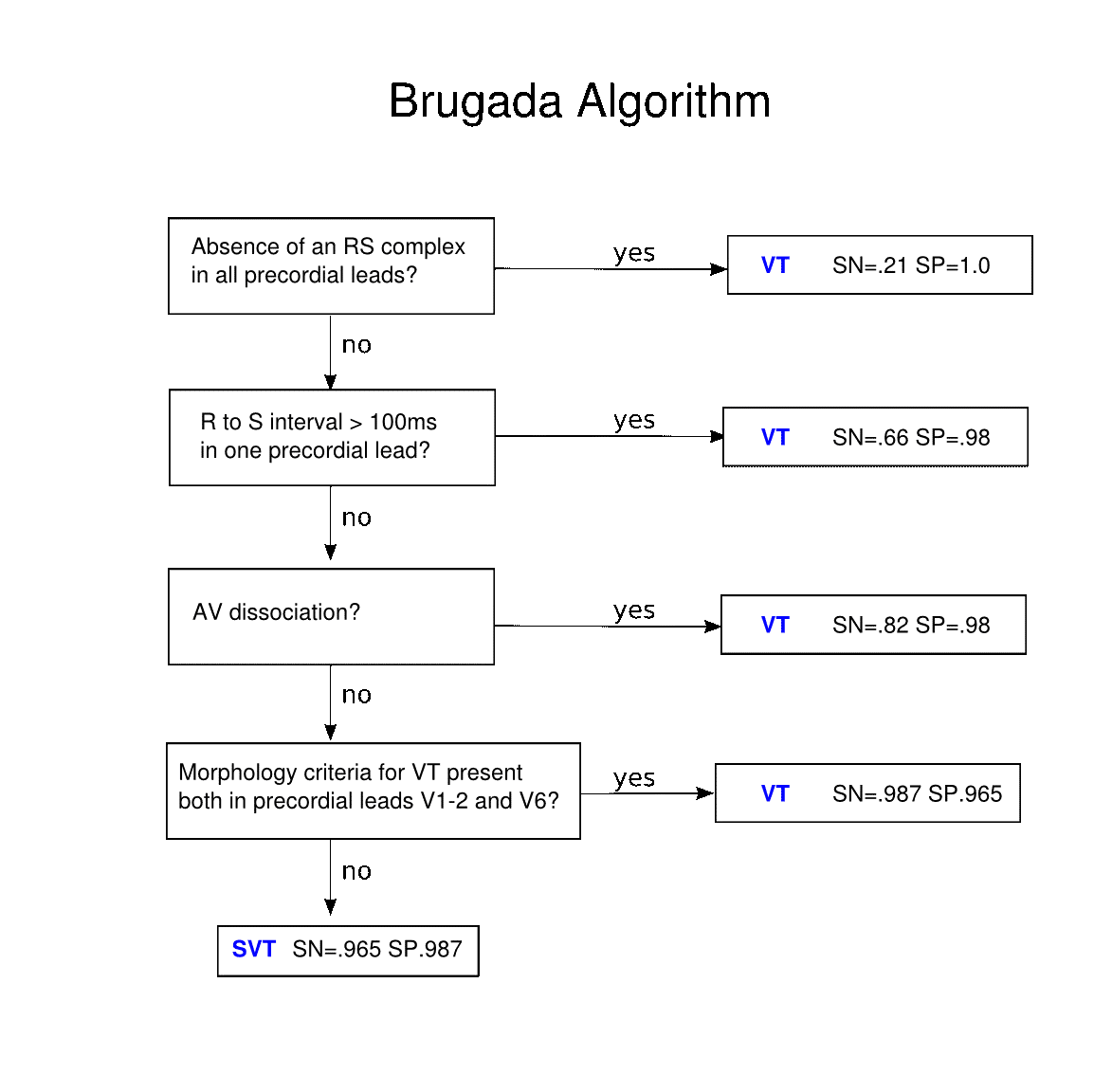
Figure 2. Brugada Algorithm for diagnosis of VT versus SVT
Assessment of the tachycardia, using the Brugada algorithm, revealed the following:
- Absence of an RS complex in all precordial leads?
No. An RS complex is present in every precordial lead.
Typically, VT presents with an absence of an RS complex in precordial leads, also referred to as chest lead concordance. Concordance exists when all QRS complexes in the chest leads are either predominantly positive or predominantly negative. The presence of concordance suggests that the tachycardia has a ventricular origin.3
- R to S interval >100ms in one precordial lead?
No. The longest RS interval is seen in V2, however this measures <100ms (Figure 3).
The RS interval is the time from the onset of the R wave to the nadir of the S wave. During SVT with aberrancy, the initial ventricular activation is fast as it occurs via the normal His-Purkinje system, whilst the conduction delay affects the terminal portion of the QRS. Conversely, during typical monomorphic VT, initial ventricular activation is slower as it spreads from myocyte-to-myocyte, bypassing the fast conduction system and resulting in a broad RS interval. 4
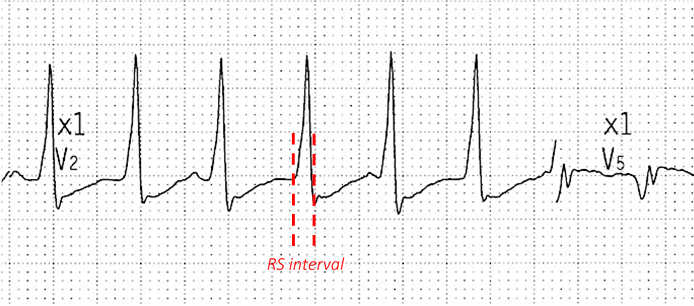
Figure 3. Measurement of the longest R to S interval in any precordial lead
- AV dissociation?
Yes. Upon careful inspection, we can see some dissociated P waves in the beats highlighted by arrows in Figure 4.
Atrioventricular (AV) dissociation describes arrhythmias where independent pacemakers control the atrial and ventricles. During SVT with aberrancy or antidromic AVRT, ventricular activation occurs via the AV node or an accessory pathway, respectively. Therefore, 1:1 conduction is a pre-requisite for arrhythmias of supraventricular origin, unless a degree of AV block is present in which the atrial rate will exceed the ventricular rate. When AV dissociation is present, in which the ventricular rate exceeds the atrial rate, VT diagnosis can be made with 100% specificity.5
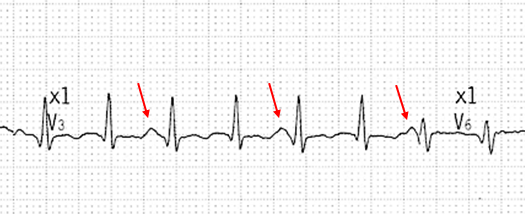
Figure 4. AV dissociation in lead V3; P waves indicated by arrows
Management
Initially, in the emergency department, this arrhythmia was diagnosed as SVT due to unobvious AV dissociation and the lack of an overtly broad QRS complex. Accordingly, 6mg of IV adenosine was given in an effort to slow AV conduction and terminate the tachycardia. However, despite multiple increasing boluses of adenosine, no change in rhythm was seen and the patient became progressively hypotensive. Upon closer inspection of the rhythm, AV dissociation was identified (as described above) and VT was classified.
The VT did not self-terminate, therefore, the patient underwent direct current cardioversion, which reverted her to normal sinus rhythm at 60bpm. A comprehensive work-up was subsequently carried out to determine potential causes of the VT. Angiography found no new significant coronary disease. Echocardiography showed moderate left ventricular systolic dysfunction with inferior wall akinesia, whilst cardiac MRI revealed a large inferior wall transmural infarct. Taken together, these results suggest that the VT is likely scar-related, in association with the patient’s previous inferior myocardial infarctions.
Later, recurrent episodes of VT occurred which lead to hemodynamic instability. The episodes were unresponsive to amiodarone infusion, and so further synchronised shocks were delivered to restore sinus rhythm. Consequently, the patient was indicated for a secondary prevention ICD to prevent further hemodynamically unstable rhythms.
Analysis of subsequent VT episodes recorded by the device confirms the diagnosis of VT due to the presence of more V-sense events than A-sense events on the EGM channels (Figure 5).
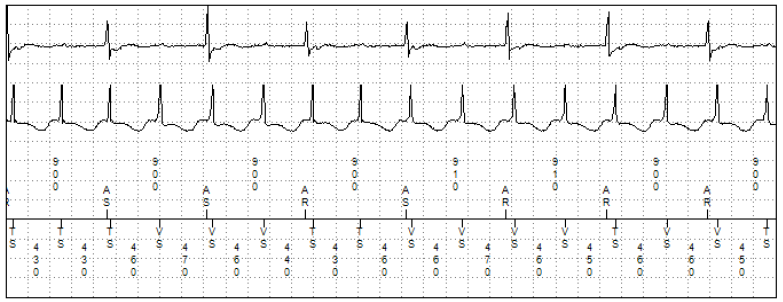
Figure 5. ICD reco
References
- Alzand B, Crijns H.Diagnostic criteria of broad QRS complex tachycardia: Decades of evolution. Europace. 2011;13(4):465-72.
- Brugada P, Brugada J, Mont L, et al. A new approach to the differential diagnosis of a regular tachycardia with a wide QRS complex. Circulation. 1991;83(5):1649-59.
- Edhouse J & Morris F. Broad complex tachycardia – Part 1. BMJ. 2002;324(7339):719-722.
- Vereckei A.Current algorithms for the diagnosis of wide QRS complex tachycardias. Curr Cardiol Rev. 2014;10(3):262-76.
- Garner J & Miller J. Wide complex tachycardia – Ventricular tachycardia or not ventricular tachycardia, that remains the question. Arrhythm Electrophysiol Rev. 2013;2(1):23-29.

