Answer
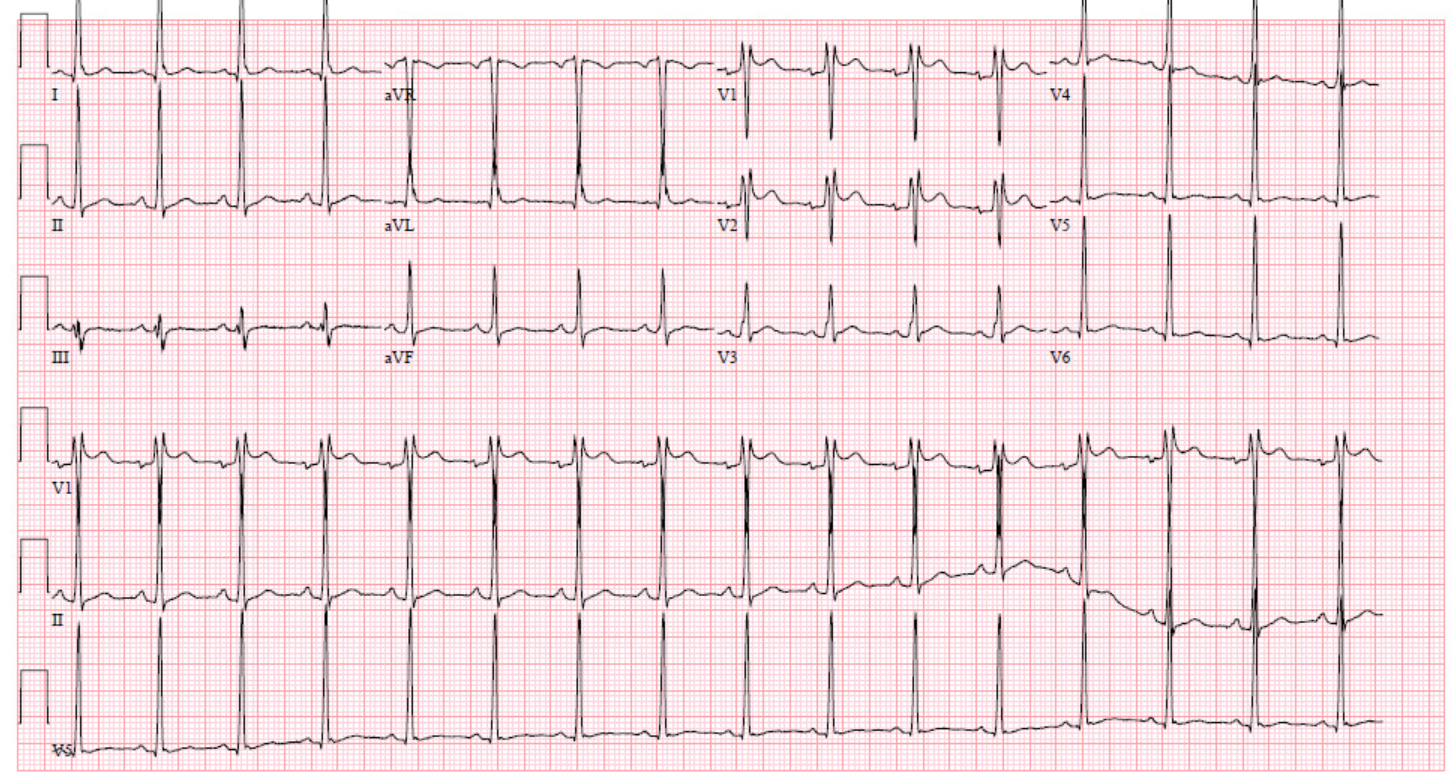
Repeat EKG
Discussion
This case reflects new onset atrial fibrillation in a young patient without evidence of structural heart disease, who has a post-conversion ECG with an rSr’ pattern in V1 and V2 concerning for a Type 2 Brugada pattern.
The differential diagnosis for a Type 2 Brugada pattern is broad, including both benign and pathological etiologies such as Brugada syndrome, arrhythmogenic right ventricular cardiomyopathy (ARVC), early repolarization, pericarditis, complete or incomplete right bundle branch block, electrolyte disturbances, or hypothermia 1, 2. While Brugada syndrome is classically associated with ventricular arrythmias, supraventricular arrythmias have been noted as well, with atrial fibrillation being the most common 3. Given the diagnostic and therapeutic implications of a diagnosis of Brugada syndrome, distinction between benign and pathological etiologies of Brugada pattern ECG findings is paramount.
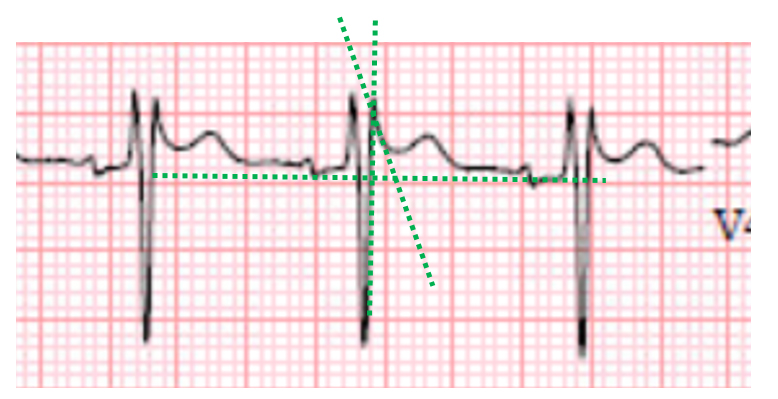
New ECG criteria to differentiate benign rSr’ patterns from Type 2 Brugada pattern have been proposed, with a particular emphasis on the downslope of the r’ wave. Specifically, a duration of greater than 4 millimeters of the base of a triangle formed by the upslope of the S wave, downslope of the r’ wave, and a horizontal line 5 millimeters below the peak of the r’ wave is suggestive of Type 2 Brugada pattern, with a specificity approximated to be 95.6% in one study 4, 5. Note that in this ECG, the base of this triangle is less than 4 millimeters in duration, reflecting a steep downslope of the r’ wave and suggesting against a Type 2 Brugada pattern (Figure 2) 5.
Given this rSr’ morphology and the fact that this ECG pattern was noted soon after spontaneous conversion to sinus rhythm with borderline tachycardia (approximately 100 bpm), a repeat ECG was obtained, with complete resolution of the Brugada pattern noted in leads V1 and V2 at a slower ventricular rate of 60 beats per minute. The patient’s negative family history of sudden cardiac death or arrythmias, lack of personal history of syncope or ventricular arrythmias, and the presence of other potential explanations for atrial fibrillation (likely undiagnosed sleep apnea, history of alcohol use) further suggested against a possible underlying diagnosis of Brugada Syndrome. As such, the patient’s ECG pattern was attributed to a transient incomplete right bundle branch block in the setting of spontaneous conversion to sinus rhythm, and further diagnostic workup for Brugada Syndrome was not pursued.
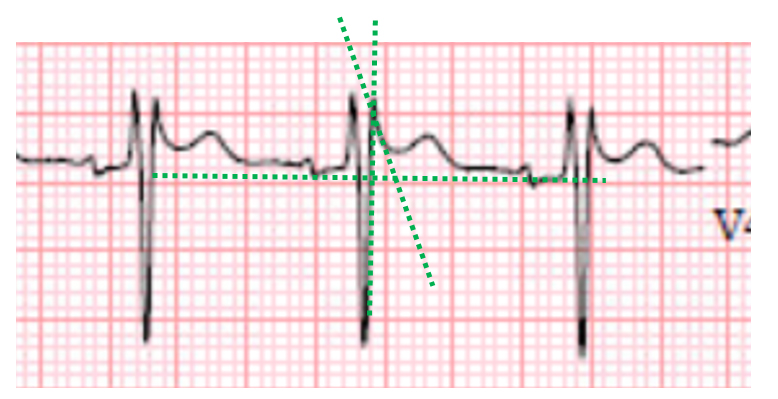
Figure 2: Closer analysis of rSr’ pattern evidenced in this patient’s ECG. Dashed green lines reflect a triangle bordered by the upslope of the S wave, downslope of the r’ wave, and a horizontal line 5 mm below the peak of the r’ wave. Note that the base of this triangle is of short duration, reflecting a steep downslope of the r’ wave, suggesting against Type 2 Brugada pattern.
References
- 1. Vohra J and Rajagopalan S. Update on the Diagnosis and Management of Brugada Syndrome. Heart Lung Circ. 2015;24:1141-8.
2. Wilde AA, Antzelevitch C, Borggrefe M, Brugada J, Brugada R, Brugada P, Corrado D, Hauer RN, Kass RS, Nademanee K, Priori SG and Towbin JA. Proposed diagnostic criteria for the Brugada syndrome: consensus report. Circulation. 2002;106:2514-9.
3. Francis J and Antzelevitch C. Atrial fibrillation and Brugada syndrome. J Am Coll Cardiol. 2008;51:1149-53.
4. Serra G, Baranchuk A, Bayes-De-Luna A, Brugada J, Goldwasser D, Capulzini L, Arazo D, Boraita A, Heras ME, Garcia-Niebla J, Elosua R, Brugada R and Brugada P. New electrocardiographic criteria to differentiate the Type-2 Brugada pattern from electrocardiogram of healthy athletes with r’-wave in leads V1/V2. Europace. 2014;16:1639-45.
5. Baranchuk A, Enriquez A, García-Niebla J, Bayés-Genís A, Villuendas R and Bayés de Luna A. Differential diagnosis of rSr’ pattern in leads V1 -V2. Comprehensive review and proposed algorithm. Annals of noninvasive electrocardiology : the official journal of the International Society for Holter and Noninvasive Electrocardiology, Inc. 2015;20:7-17.