October 2023
Change in EP EGM – What is the cause?
Phil Matthews Highly Specialist Cardiac Physiologist, Golden Jubilee University National Hospital, UK
Disclosure: The author has no conflict of interests to declare.
Background
A 51-year-old male patient was referred for a Cryo Pulmonary Vein Isolation (PVI) ablation procedure due to documented paroxysmal Atrial Fibrillation (pAF). Previously he had noted palpitations for several years and after commencing Sotalol 80mg bd, he felt that he was in sinus rhythm the majority of the time although with occasional short-lived episodes of palpitations. Regarding his lifestyle, he is an ex-smoker after cessation 5 years prior, does not drink caffeine but does drink up to 6 pints of beer on weekend evenings. Echocardiogram showed a structurally normal heart with no significant left atrial dilatation. Medical history includes musculoskeletal back pain which is controlled by Tramadol prn and depression which the patient takes Fluoxetine 20mg od. Due to potential interactions between Fluoxetine and Sotalol causing prolonged QT segments, the patient was offered the option of alternative anti-arrhythmic medications or the option of catheter ablation.
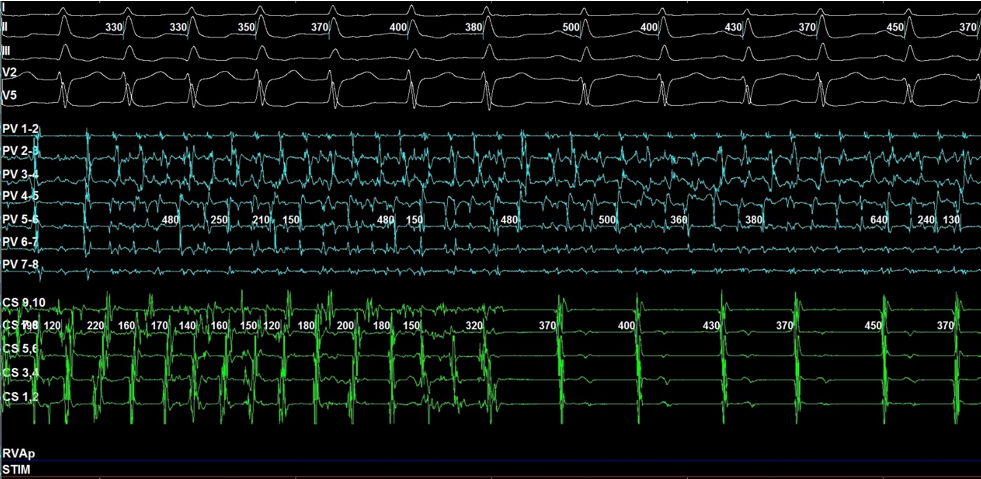
Cryo PVI was undertaken with 2 catheters, a SJM Inquiry Coronary Sinus catheter and a Medtronic Achieve Pulmonary Vein catheter. During the first application of cryoablation treatment to the Left Superior Pulmonary Vein (LSPV), the following EGM (sweep speed 100mm/sec) was captured 50 seconds from onset of treatment and 5 seconds after balloon temperature reached -40C: –
QUESTION
What can be seen in the captured EGM?
Disclaimer: The British Heart Rhythm Society (BHRS) collates submissions for the ECG/EGM challenge on this website. These submissions, along with any accompanying answers, are provided by external contributors and are published for informational purposes only. BHRS does not endorse, guarantee, or warrant the accuracy, completeness, or reliability of any submissions or answers provided.

