Answer
Repetitive non-reentrant VA synchrony (RNRVAS)
Explanation
Repetitive non-reentrant VA synchrony (RNRVAS) is a device related arrhythmia similar to pacemaker mediated tachycardia (PMT) although is usually seen at slower rates than a PMT. It is a repetitive sequence of ventricular pacing (VP) with retrograde conduction, functional undersensing of the retrograde P wave, functional loss of capture of the next delivered atrial pace (AP) with the next VP with subsequent VA conduction setting off the sequence again.
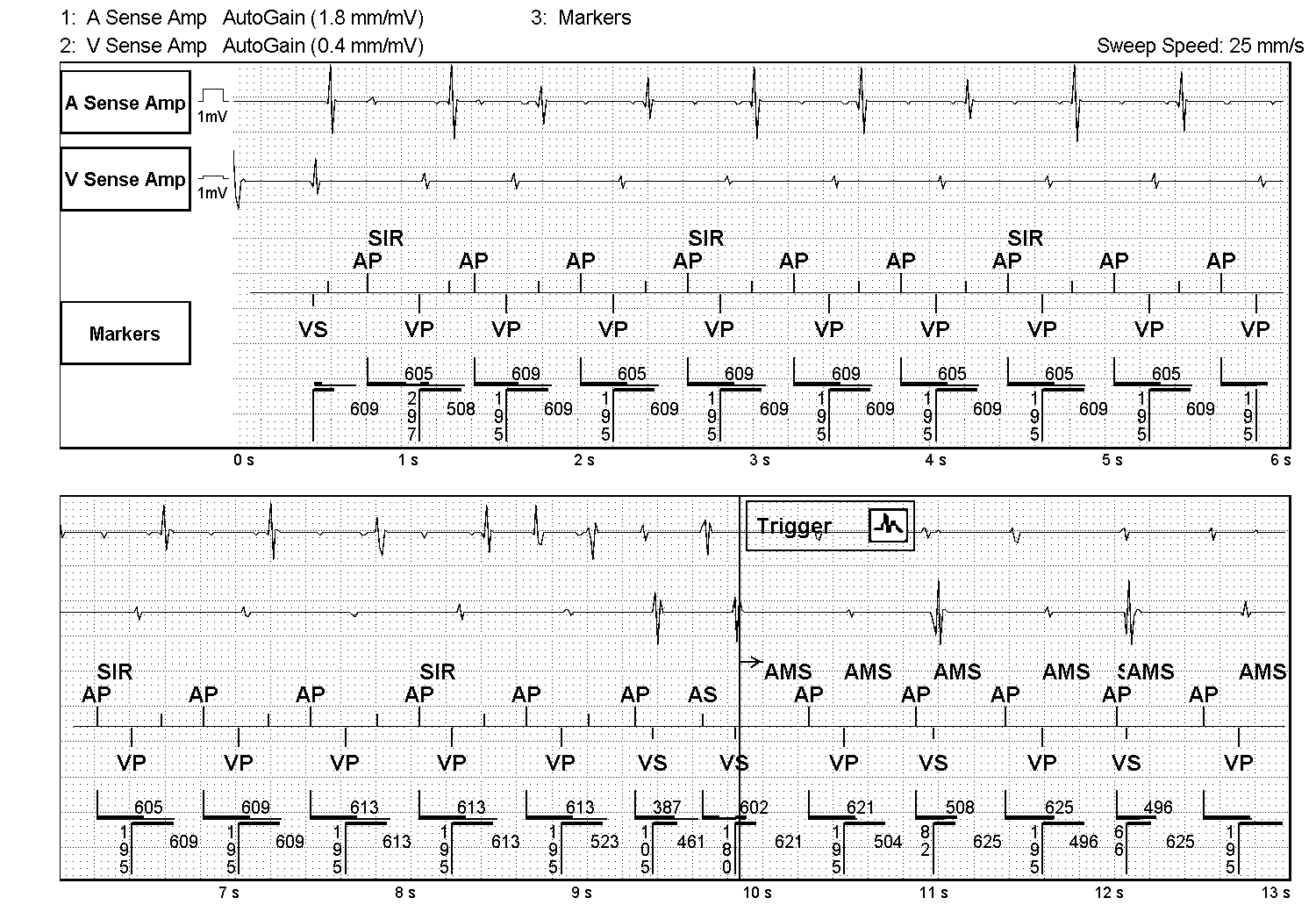
In the trace in figure 1 the episode of RNRVAS is likely to be caused by a combination of one long AV interval due to VIP programming and sensor driven atrial pacing with the trigger a premature ventricular contraction (PVC). The PVC occurs just before an atrial event (possibly an intrinsic P wave). The atrial event is marked by a short vertical line on the atrial side of the marker channel indicating an atrial event falling in the post ventricular atrial refractory period (PVARP). This functionally undersensed atrial event is ignored by device timings and the atrial escape interval times out with an AP delivered, driven by the sensor rate (SIR). The AP has functional loss of capture as the atrium remains in refractory from the initial atrial event. The AP triggers an AV interval (AVI) which for one cycle is long at 300ms due to VIP programming. With no antegrade AV conduction the AVI times out, a VP is delivered with retrograde VA conduction and the sequence of functional atrial undersensing, functional loss of atrial capture and ventricular pacing with retrograde conduction starts, only this time with the shorter paced AV delay of ~200 bpm.
Development of RNRVAS is favoured in devices programmed with a high base rate, long AV delays, a long PVARP and with sensor driven pacing. It can be responsible for patient symptoms consistent with pacemaker syndrome and has been reported to trigger atrial fibrillation (AF) in some patients. It can occur in dual and triple chamber devices when VA conduction is intact and is seen in tracking (P synchronous ventricular pacing) and non-tracking modes that allow AV-sequential pacing (DDI, DDIR).
Anecdotally it is most commonly observed in Abbott devices recorded as an AMS episode as the Abbott AMS algorithm counts AP events towards the mode switch trigger count but it is possible with all manufacturer devices.
Programming features that increase the atrial escape interval can be used to help eliminate RNRVAS. Shortening the AV delays (turning off VIP in this instance), reducing the base rate and adjusting the maximal sensor rate can be used as programming fixes to this device related arrhythmia. These programming changes result in, the atrial paced events falling when the atria are no longer refractory and therefore capture the atrial myocardium.
A few device manufacturer specific algorithms may also help eliminate RNRVAS including turning on AP on PVC response algorithm in Abbott devices when a PVC is the trigger of RNRVAS. Using non-competitive atrial pacing (NCAP) programmed at 300 to 400ms in Medtronic devices may also prevent the rhythm from occurring.